Partnering with providers to advance care innovation
Like most healthcare executives, Mark Clement, the CEO of Cincinnati-based health system TriHealth, looks for ways to get healthcare right through the “Triple Aim” of better health, better care, and better value.
 Mark Clement, CEO of TriHealth
Mark Clement, CEO of TriHealth
“Over time, this is going to bend the cost curve by delivering on the Triple Aim. Working with Anthem, we’ve already demonstrated it in delivering more efficient care.” — Mark Clement, CEO of TriHealth
Working closely with Anthem Blue Cross and Blue Shield of Ohio, Mark’s team has been improving the quality of care for thousands of patients while lowering costs for employers—including TriHealth itself. Key to their success: Anthem’s centerpiece value-based care program, called Enhanced Personal Health Care, which provides market-leading data sharing with TriHealth’s population health team to flag gaps in care, opportunities for process improvement, and cost savings for patients.
“We’ve been able to show dramatic reductions in healthcare costs for our own 12,000 employees, while improving their health and productivity,” Mark says. “It really does work.” Enhanced Personal Health Care (EPHC) shifts spending from a traditional “fee for service” approach to one that promotes prevention and care coordination. Primary care providers at participating health systems, such as TriHealth, gain access to advanced analytics that help them pinpoint the patients who can benefit from interventions, better manage chronic conditions, and identify gaps in care that can have serious health ramifications.
The Anthem-TriHealth partnership, which began in 2014, supports primary care providers through payment incentives used in coordinating, planning and managing patient care. A portion of the cost savings is returned to TriHealth, which can then be invested in preventive health and chronic disease management programs, as well as care management and coordination. Anthem returns another portion of the savings to employers, and the remaining cost savings help control increases in health insurance premiums.
“Without the incentives and support we received from EPHC, we wouldn’t have been able to enhance our operations the way we have.”— Jennifer Sharp-Warthan, M.D., Medical Director of Tidewater Physicians Multispecialty Group in Virginia
Leadership in value-based care
Approximately 66 percent of Anthem’s total medical spend is tied to payment innovation programs, and EPHC is among the largest private value-based payment program in the country for providers participating in commercial, Medicare and Medicaid segments. EPHC now includes 166 accountable care organizations and 87,000 providers. And under the standard Commercial EPHC program, providers manage 6.3 million lives and have, since 2014, accumulated $1.8 billion in gross savings for Anthem clients across the country.
“Over time, this is going to bend the cost curve by delivering on the Triple Aim,” Mark says. “Working with Anthem, we’ve already demonstrated it in delivering more efficient care.”
Medical cost increases for the 90,000 TriHealth patients insured by Anthem are less than half the typical industry rates. But the lower cost is just part of the success story. Many of the people insured by Anthem who receive care through TriHealth are taking advantage of preventive care, including children’s annual checkups, diabetes testing and management, and vaccinations—making TriHealth among the best Accountable Care Organizations in the country, as reflected in their quality of care results:
- 93% for well-child
immunizations - 79% for breast cancer
screenings - 79% for diabetic
complication screenings - 78% for medication
adherence
 Mark and TriHealth certified medical assistant discuss the positive results of value-based care
Mark and TriHealth certified medical assistant discuss the positive results of value-based care
“Value-based care is a win for everyone—for businesses, for communities, for our nation’s health systems, and, most importantly, for the individuals who entrust their health to us,” said Clement. “It truly is the right thing to do.”
TriHealth is far from alone in understanding the importance of value-based care. Enhanced Personal Health Care providers across the country credit EPHC with creating a path to success under value-based care. “Without the incentives and support we received from EPHC, we wouldn’t have been able to enhance our operations the way we have,” says Jennifer Sharp-Warthan, M.D., Medical Director of Tidewater Physicians Multispecialty Group in Virginia.
Now Anthem is taking EPHC to the next level by creating a new payment model and product called Cooperative Care—a program designed to deliver a markedly better consumer experience by relying on a high-performing network of providers.
 Deepti Jain, leader of IngenioRx, Anthem’s new pharmacy benefits organization
Deepti Jain, leader of IngenioRx, Anthem’s new pharmacy benefits organization Deepti discusses IngenioRx’s mobile and desktop applications, which allow consumers to access pharmacy and medical information in a single location
Deepti discusses IngenioRx’s mobile and desktop applications, which allow consumers to access pharmacy and medical information in a single location Erik Sossa, PepsiCo’s Vice President for Global Benefits and Wellness
Erik Sossa, PepsiCo’s Vice President for Global Benefits and Wellness Rajeev Ronanki, Anthem’s Chief Digital Officer
Rajeev Ronanki, Anthem’s Chief Digital Officer Rose and Joseph enjoy time together, prior to Joseph’s mounting health challenges
Rose and Joseph enjoy time together, prior to Joseph’s mounting health challenges Rose with an Aspire social worker, who provided needed support and comfort
Rose with an Aspire social worker, who provided needed support and comfort Ronald reunited with his son
Ronald reunited with his son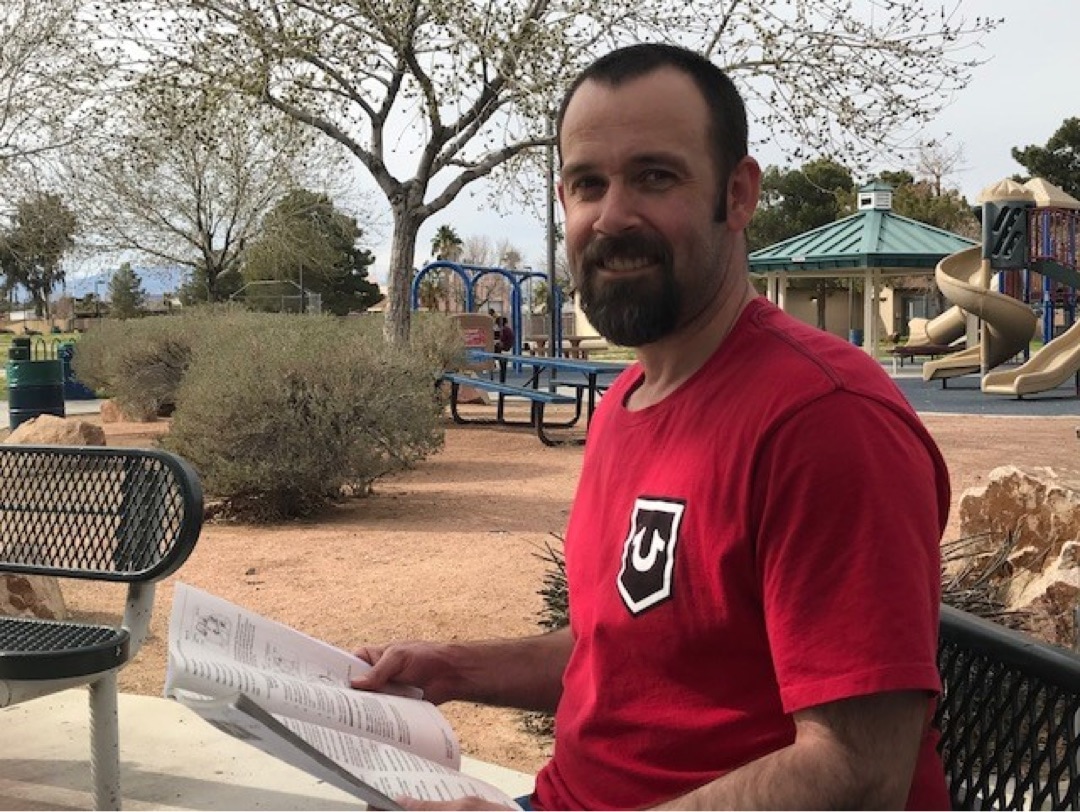 Supported by Pathways Forward, Ronald studies for his commercial driver’s license
Supported by Pathways Forward, Ronald studies for his commercial driver’s license Dr. David C. Ardaya has identified diabetes through routine eye exams and alerted other care providers on the Whole Health Connection platform
Dr. David C. Ardaya has identified diabetes through routine eye exams and alerted other care providers on the Whole Health Connection platform Leah Vice, Anthem nurse case manager
Leah Vice, Anthem nurse case manager Carolyn Barbieri, participant in the Aging Mastery Program, says it “was one of the best things I’ve ever done”
Carolyn Barbieri, participant in the Aging Mastery Program, says it “was one of the best things I’ve ever done” Jeraud Ferguson, Anthem associate and founder of Each One, Teach One AWOL (A Way of Life), a youth development program
Jeraud Ferguson, Anthem associate and founder of Each One, Teach One AWOL (A Way of Life), a youth development program Anthem associates volunteering at Indiana School for the Blind during Anthem Volunteer Days
Anthem associates volunteering at Indiana School for the Blind during Anthem Volunteer Days Andrew Piske, an Anthem associate and former firefighter, with his K-9 rescue partner, Maddy
Andrew Piske, an Anthem associate and former firefighter, with his K-9 rescue partner, Maddy I. Steven Udvarhelyi, M.D., President & CEO of Blue Cross and Blue Shield of Louisiana
I. Steven Udvarhelyi, M.D., President & CEO of Blue Cross and Blue Shield of Louisiana Dr. Udvarhelyi with Aaron Lambert, President of Healthy Blue
Dr. Udvarhelyi with Aaron Lambert, President of Healthy Blue